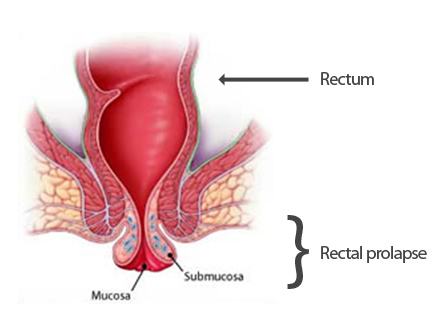
Rectal prolapse
What is a rectal prolapse?
A rectal prolapse is a condition in which the lower part of the rectum or the mucosa of the rectum is squeezed out through the anus. In the presence of a rectal prolapse there is often reduced strength in the sphincter muscle resulting in additional symptoms such as mucus secretion and mild degrees of fecal incontinence. Although much more common in women rectal prolapse can affect both sexes.
What causes a rectal prolapse?
Many factors may play a part in the development of a rectal prolapse. A prolapse may occur as a result of chronic constipation and straining during bowel movement. A prolapse may occur as a complication to difficult childbirth during which the sphincter muscle might become injured or lacerated. Furthermore there is an age-related cause as the muscles throughout the body become weaker with age and thus also in the pelvis and pelvic floor on which or through which the uterus, urinary bladder and rectum can descend. Rarely one single reason for rectal prolapse can be pinpointed.
Is a rectal prolapse the same as hemorrhoids?
A rectal prolapse can be mistaken for hemorrhoids, as some symptoms are identical: bleeding, maybe pain and tissue appearing through the anus. Often however a rectal prolapse will result in leakage of mucus and small amounts of feces, which is rarely the case with hemorrhoids. A rectal prolapse consists of the mucosa or bowel wall in contrast to hemorrhoids, which are a kind of varicose veins/varices or dilated blood vessels in the anal canal.
How is the diagnosis made?
A specialist in gastroenterology and/or colorectal surgery can quite easily make the diagnosis based on the symptoms and a simple examination of the rectum. It can be necessary to squeeze or strain to provoke the prolapse.
If the prolapse occurs inside the rectum and does not protrude through the anal opening it can be more difficult to make the correct diagnosis. In this situation it might be necessary to conduct additional examinations in a hospital setting (x-ray, scan, manometry).
These examinations also are also decisive as to which treatment is optimal in the individual situation.
How is a rectal prolapse treated?
Even though constipation and straining during bowel movement is often contributing to the development of rectal prolapse it is rarely sufficient to correct the consistency of the feces and bathroom habits once the prolapse is present.
Some kind of operation or surgical intervention is most likely to be necessary.
In the case of prolapse of the mucosa the problem can often be corrected by rubber band ligation in the same way internal hemorrhoids are treated (see info on rubber band ligation of hemorrhoids) or by removal of the mucosa under local anesthesia.
If a larger prolapse is present it can be necessary to perform an operation (laparoscopy) under general anesthesia during which the rectum is lifted back into the pelvis and attached to the pelvic wall/sacrum.
Is treatment successful?
The major part of these conditions can be corrected to a point where the majority of patients become symptom-free or have only minimal discomfort. The results depend on whether the sphincter muscle is intact and can be restored/trained to normal strength. It might take a year to train a sphincter muscle that has been stretched by a prolapse. Cronic constipation and straining during bowel movement must be avoided.